By Dr Brenda Baker BDS (Syd.) Hons. MSc Conservative Dentistry (London) Southern Cross Dental.
A diversity of clinical situations present to the practitioner. Two interesting case studies are reviewed in the following article. One case study reviews implant-supported overdentures which are becoming a more commonplace treatment modality as patients seek options to enhance masticatory efficiency and comfort. The other case study examines root resorption and possible aetiological factors which contribute to the phenomenon.
Implant-supported overdentures
An implant-retained overdenture may be indicated in patients with changed anatomy, neuromuscular disorders, significant gag reflex or considerable ridge resorption (Vere J. et al., 2012). Implantretained overdentures may reduce residual ridge resorption and enhance mastication and hence nutritional status, improve speech and patient selfesteem (Doundoulakis JH. et al, 2003). Overdentures may be retained by a number of different implants, which can be splinted or freestanding (Dudic, A. and Merickse-Stern, R., 2002). Authors have reported high implant survival rates for mandibular overdentures, and thus successful treatment outcomes, when overdentures are retained by two implants (Meijer HJ. et al, 2009) either splinted or non-splinted. In the maxilla, the evidence base supports the use of four to six implants splinted with a bar, although freestanding abutments are increasing in popularity (Galluci GO. et al., 2008).
Various prosthetic options and attachments are available:
1. Bar and clip systems
The major bar types come with matching clips. The use of the spacer enables a space between the clip and the bar when the prosthesis is at rest in the patient’s mouth. Upon biting, the denture is capable of some vertical movement so that there is some support for occlusal loads instead of purely implant support. Milled bars do not allow movement of the denture base and can provide relief over painful areas such as a superficial mental nerve (Dudic, A. and Merickse-Stern, R., 2002). A cast bar may be made including proprietary components, or a custom design can be fabricated. Subsequently, the denture is made to fit over the custom design.
Both rigid and resilient bars can be used to align non-parallel implants. However, they need at least 10 mm of interocclusal clearance and should not be used when vertical space is limited (Chee, W. and Jivraj, S., 2006).
2. Studs
All stud attachments should be parallel to each other and the attachments should not interfere with the insertion path of the overdenture.
3. Magnets
Magnets provide the least retention.
4. Telescopic copings (rigid and non-rigid)
Note that patients with advanced resorption of the ridge are suitable for bar or telescopic attachment assemblies that offer horizontal stability. Patients with minimal alveolar resorption of the ridge are suitable for studs or magnetic attachment assemblies.
Case Study I
This patient initially presented with both upper laterals fractured at the gum line (Fig. 1).
Teeth 26 and 24 were missing. Intraoral examination indicated evidence of generalised moderate to severe periodontitis.
The following options were discussed with the patient:
1. Full denture


2. Partial denture
3. Bar-retained full denture.
4. Replacement of missing / unrestorable teeth with implant/ crowns.
The patient decided on option 4 with a view of option 3 in the future.
The surgical procedure proceeded uneventfully. The laterals were extracted. Implants surgery was then carried out 6 weeks later. The laterals were replaced with 4mm x 12mm Parallel BioHorizons implants.
A 3.5mm x 12mm implant was placed in the 24 area and a 5.0 x 12mm implant in the 16 area. A temporary bridge was then constructed using the canines and centrals as abutments. Two weeks postsurgery the patient complained of pain in the 12 implant area. An intra-oral exam revealed fluctuant swelling in the buccal tissues apical to tooth 11. A periapical radiography revealed periapical pathology and a decision was made to remove tooth 11. The patient then made a decision to have all remaining teeth removed and implement option 3. A week later, implant 12 failed to integrate and became loose. It was clear that the infection from the 11 had compromised the adjacent implant.
In consultation with the technician, the dentist decided to make an immediate full upper denture. Subsequently all remaining teeth, 18, 17, 15, 14, 13, 23, 25 were extracted and the full upper denture inserted (Fig. 2).
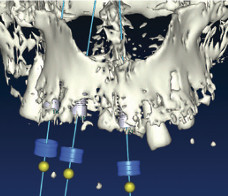
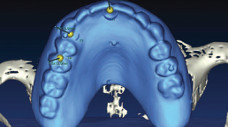
After three months, following uneventful healing, a replica of the full upper denture was made with clear cold cured acrylic and 6 radiographic markers placed. A CT scan was made of the maxilla with the Radiographic Guide in Place. The Guide was then scanned on its own in a soft tissue window. Using software, the two scans were merged using the radiographic markers to align the images (Figs. 3-5). Three more implants were then planned to provide the required six implant support. The new implants were then inserted in the 11, 13 and 15 position. An external sinus lift was offered to the patient so that a 16 implant could be placed but the patient was strongly against any type of invasive surgery.



An internal lift was not possible due to a very uneven sinus floor making a perforation a probable scenario. It was decided that a cantilever bar to the 16 area was a good compromise considering that there were six implants in total.
After a further three months post implant surgery, a review appointment revealed the recent implants had all successfully integrated. An open special tray final impression was taken after the implants were rigidly fixed together. A custom milled bar was then manufactured by the laboratory and tried in for passive seating (Fig. 6).
An excellent result was obtained (Fig. 7). On confirmation of passive seating of the bar, an acrylic/ wax plate was made using three implants as an anchor point. This enabled a precise interocclusal registration to be carried out. The laboratory then finished the case by make a Co-Cr upper full denture without any palatal coverage. The milled bar was torqued down to the 30Ncm level and the plate inserted over it (Fig. 8). Excellent retention and aesthetics were obtained (Fig. 9).
Clear instructions were given to the patient on how to clean around and underneath the bar. A review appointment two weeks after insertion of the final prosthesis revealed the patient was maintaining excellent oral hygiene. A slight bite adjustment was made on a premature posterior contact. The patient was delighted with the final aesthetics. Root resorption The aetiology for resorption starts from injuries to the tooth, including thermal, mechanical and chemical (Nilsson E. et al., 2013) factors. Pathologic resorption can also occur from orthodontic tooth movement or from chronic infections of the pulp or periodontal tissues (Ne RF. et al., 1999). Root resorption may be classified based on its location in relation to the root surface: external root resorption (ERR) and internal root resorption (IRR). ERR is resorption that starts in the periodontium and initially affects the external surfaces of a tooth. It can be further classified as surface, inflammatory, replacement, or by location as cervical, lateral, or apical. It may or may not invade the dental pulp space (www.aae.org/glossary). IRR is an inflammatory process which starts within the pulp space with loss of dentine and possible invasion of cementum (www.aae.org/glossary). IRR is rare compared with ERR.
The pathogenesis of resorption will now be revised. Osteoclasts are multinucleated giant cells which cause bone resorption. The pathology of IRR is caused by transformation of normal pulp tissue into granulomatous tissues with osteoclasts, which resorb dentine. This, in turn, resorbs the dentinal walls, advancing from the centre to the periphery. There are two types of IRR: internal inflammatory resorption and internal replacement resorption. Inflammatory resorption– the resorptive process occurs if the intraradicular dentine progresses without adjunctive deposition of hard tissues adjacent to the resorptive sites. The phenomenon is associated with the presence of granulation tissue in the resorbed area and is identifiable with routine radiographs as a radio-clear zone centered on the root canal.


Replacement resorption– the resorptive activity causes defects in the dentine adjacent to the root canal, with concomitant deposition of bone-like tissue in some regions of the defect. An irregular enlargement of the pulp space with partial or full obliteration of the area of the pulp chamber occurs. CBCT has allowed more precise and complete diagnosis of IRR and ERR and is highly advised in early presentations of potential resorption (Nilsson E. et al., 2013).
IRR is usually asymptomatic, but pain or discomfort may be the chief complaint if the granulation tissue has been exposed to oral fluids. The granulation tissue can clinically manifest itself as a “pink spot” where the crown dentine destruction is severe. (Simmons SL., 2014). Teeth with IRR test normally to pulpal and periapical tests until the lesion grows significantly in size, which then results in perforation (Walton, R.E. and Torabinejad, M., 1996.). Once necrosis of the pulpal tissue takes place, then the typical signs/symptoms of an abscess may occur.
Case Study II
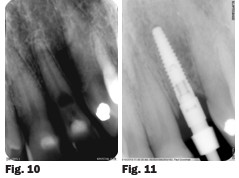
A healthy 65 year-old male presented to the surgery with the chief complaint of a loose front tooth which was uncomfortable upon chewing and with pressure. A radiograph revealed significant bone loss around tooth 22 in addition to the focalised loss of internal tooth structure in the mid-third of the root (Fig. 10). The root was almost perforated. Clinical examination revealed Class III mobility. No drainage point or fistula were noted. A diagnosis of internal resorption was given due to the focal point of radiolucency within the pulp chamber area. Due to the extent of the defect and the advanced bone loss, tooth removal was advised.
Two days later, the patient called the practice to advise that the tooth crown had completely severed. An immediate flexible partial denture was fabricated for aesthetics and surgical removal of the tooth was planned followed by replacement with an implant.
Nobel Biocare Replace Select Narrow platform was selected by the oral surgeon which was placed in the position of tooth 22 under local anaesthetic. Bone quality was good and the implant was seated to 35Ncm. The implant was placed and a screw-retained restoration was planned. The implant was submerged during the healing phase and the removable partial denture was adjusted. The periodontist placed a 5mm healing abutment. Possible minor soft tissue augmentation was to be evaluated at that time. An appointment was scheduled for 3 months later with the periodontist. At that time the periodontist reported that the implant had integrated. An impression coping was employed using an open-tray impression technique (Fig. 11).
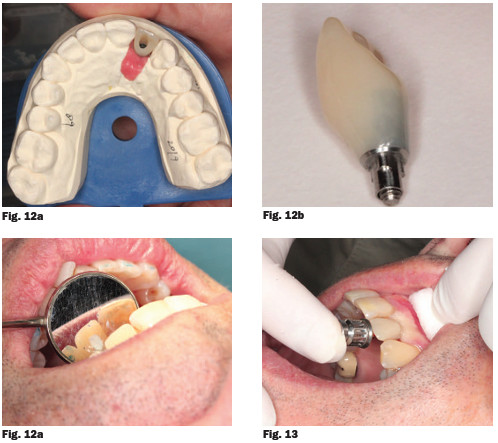
In order to achieve excellent soft tissue contours, a provisional screw-retained temporary crown on a titanium base with a hybrid-ceramic was fabricated and left in situ for 2 months (Fig. 12a, 12b and 12c). After two months, a screw-retained porcelain-fused-to-metal restoration was issued and the crown torqued to 32Ncm (Fig. 13).
Southern Cross Dental would like to thank Dr Cameron Castle, Bundaberg, Queensland for his case submission on overdentures, and Dr Albert Sharp of Double Bay, NSW for his case submission on root resorption.
References:
American Association of Endodontics, “Glossary of endodontic terms,” 2014. www.aae.org/ glossary
Chee, W. and Jivraj, S., 2006. Screw versus cemented implant supported restorations. British dental journal, 201(8), pp.501-507.
Doundoulakis, J.H., ECKERT, S.E., LINDQUIST, C.C. and JEFFCOAT, M.K., 2003. The implant-supported overdenture as an alternative to the complete mandibular denture. The Journal of the American Dental Association, 134(11), pp.1455-1458.
Dudic, A. and Mericske-Stern, R., 2002. Retention Mechanisms and Prosthetic Complications of Implant-Supported Mandibular Overdentures: Long-Term Results. Clinical implant dentistry and related research, 4(4), pp.212-219.
Gallucci, G.O., Morton, D. and Weber, H.P., 2009. Loading protocols for dental implants in edentulous patients. International Journal of Oral & Maxillofacial Implants, 24.
Meijer, H.J., Raghoebar, G.M., Batenburg, R.H., Visser, A. and Vissink, A., 2009. Mandibular overdentures supported by two or four endosseous implants: a 10-year clinical trial. Clinical Oral Implants Research, 20(7), pp.722-728.
Nilsson, Elisabeth, Eric Bonte, François Bayet, and Jean-Jacques Lasfargues. “Management of Internal Root Resorption on Permanent Teeth.” International journal of dentistry 2013.
Ne, Rita F., David E. Witherspoon, and James L. Gutmann. “Tooth resorption.” Quintessence International-English Edition- 30 (1999): 9-26.
Simmons SL. http://www.dentistryiq.com/ articles/2014/09/internal-resorption-a-briefreview-and-case-report.html
Vere, J., Hall, D., Patel, R. and Wragg, P., 2012. Prosthodontic maintenance requirements of implant-retained overdentures using the locator attachment system. International Journal of Prosthodontics, 25(4).
Walton, R.E. and Torabinejad, M., 1996. Principles and practice of endodontics.

